PTSD Diagnosis in Minutes, not Months
Earlier this summer, people around the United States set off fireworks to celebrate Independence Day. Though such colorful explosions are meant to be festive, they can also trigger distressing flashbacks in Americans who have experienced gun violence or bombings, including thousands of military veterans.
People who go through life-threatening events sometimes develop a long-term mental illness known as post-traumatic stress disorder (PTSD). According to the US Department of Veterans Affairs (VA), about six percent of Americans—including nearly 30 percent of military veterans deployed to active war zones—will experience PTSD.
PTSD diagnosis is currently highly subjective, relying on a patient’s willingness to open up about past trauma and ability to accurately self-report their symptoms.

“With PTSD, diagnosis is complicated. Every patient’s condition is different,” said Jayne Wu, a professor in the Min H. Kao Department of Electrical Engineering and Computer Science (EECS) at the University of Tennessee’s Tickle College of Engineering (TCE).
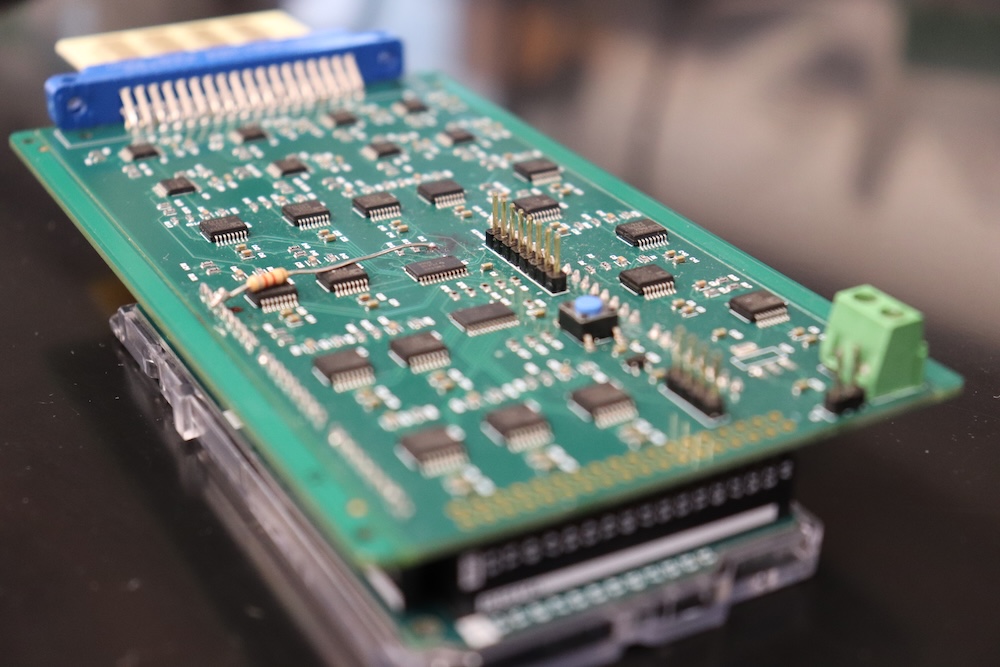
Wu, an expert in microelectronics and microfluidics, wants to create a generalized biosensor that can be used to objectively diagnose complex diseases like PTSD. She and UT Institute of Agriculture Professor Shigetoshi Eda have spent the last 14 years developing AiCAP—a patented biosensor array with the unique ability to simultaneously identify a wide range of biomarkers, which are molecules in the body that indicate the presence of a disease.
In 2023, the duo was contacted by CFD Research Corporation, a technology development organization working with the US military to create a low-cost, minimally invasive diagnostic tool for PTSD. The research group knew AiCAP was the key.
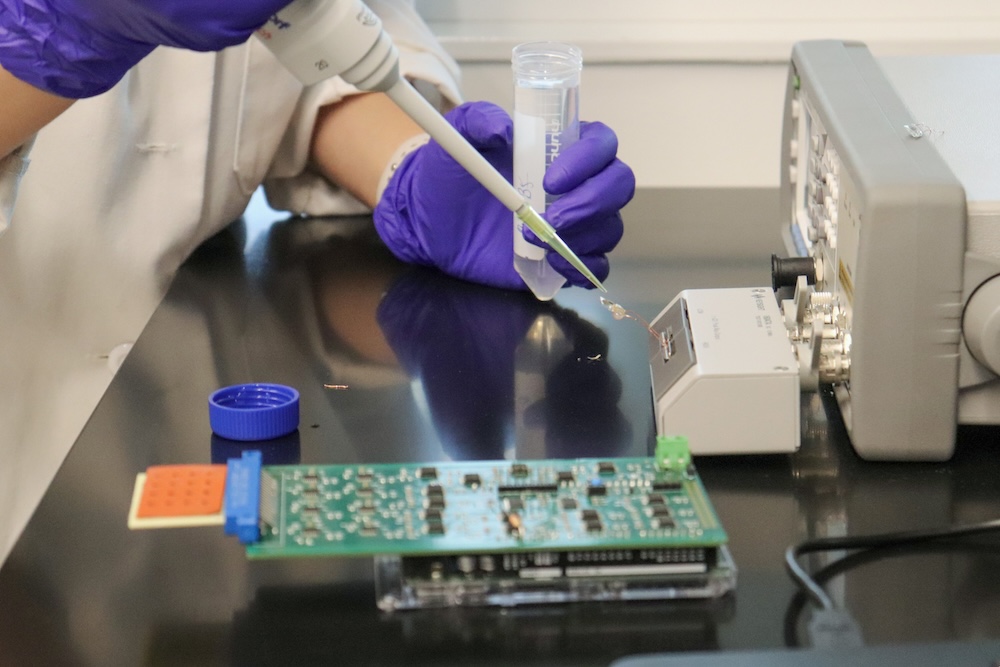
Wu, Eda, and CFD Primary Investigator David Gaddes have created a sensor which incorporates AiCAP and can already identify more than a dozen PTSD-related biomarkers from a single blood sample. They are hoping to achieve FDA approval, then expand the technology to diagnose other diseases like traumatic brain injury, cancer, sepsis, and organ damage.
“PTSD is a great example to demonstrate the potential benefits of our sensor array in furthering precision (personalized) medicine,” Wu said.
University Innovations and Industry Expertise
Unlike the flu, PTSD does not have a single diagnostic biomarker. Dozens of biomarkers are associated with PTSD, including proteins, nucleic acids like DNA, fats, and carbohydrates.
“Usually, you need different detector for each type of biomarker,” Eda said. “Jayne’s approach within AiCAP allows you to detect different types of biomarkers using a single device.”

That’s a major boost to multi-omics, the simultaneous study of many types of biological molecules, and it’s applicable in many domains. Wu and Eda’s team previously deployed a handheld version of AiCAP that can diagnose diseases in dairy herds, delivering a diagnosis from a sample of milk or serum within minutes.
However, tailoring the multi-omics sensor to a human medical setting and scaling production so the device can be deployed quickly once it has FDA approval required CFD’s development capabilities.
“It’s very valuable for industry and university researchers to collaborate,” Gaddes said. “University researchers are coming up with technologies that are new, or which have new applications, and demonstrating that they work. Companies like CFD can then come in and develop the technology into an actual product.”
Getting AiCAP into Clinics
Wu and Eda have always made broad availability a cornerstone of AiCAP’s development.
“For technology to reach into every corner of our society, you need to make it accessible at every level,” Wu said.
To achieve the widespread use the team is hoping for, the research team has kept the multi-omics sensor handheld and inexpensive. They are also working on a user-friendly, intelligent read-out system that shows both the raw test results and a holistic readout that simplifies data interpretation. That way, a PTSD diagnosis could come directly from a family physician without going through an offsite specialist or engineer.
“We’re hoping that this would be the first multi-omic point-of-care biosensor,” Gaddes explained. “That means it’s something that’s very easy for a doctor to run and operate—they put a sample in, they get an answer out.”
Gaddes presented the team’s sensor at the Military Health System Research Symposium in Orlando, Florida, in October 2024. The sensor was very well received, with multiple attendees asking to help prototype the device or be alerted as soon as it becomes commercially available.
“What I’m excited about on this particular project is the ability to do fast multi-omic sensing,” said Gaddes. “From a less technological standpoint, I’m excited about making a product which improves the diagnoses of complex diseases like PTSD.”
Contact
Izzie Gall (865-974-7203, egall4@utk.edu)
